
Is Snoring a Medical Condition?
“Laugh, and the world laughs with you; snore, and you sleep alone.” – Anthony Burgess
It’s well known that good sleep is crucial for maintaining both physical and mental health. Sleep disorders not only result in poor sleep quality, daytime fatigue, and drowsiness, but they are also associated with numerous diseases such as hypertension, diabetes, and stroke. One of the most common causes of sleep disturbances is obstructive sleep apnea (OSA), often characterized by snoring. According to data, approximately 20 million people in the United States suffer from sleep apnea, yet about 75% of them may not even be aware they have the condition. This is particularly significant for men, as they are twice as likely as women to have sleep apnea.
Obstructive Sleep Apnea (OSA) Causes, Symptoms, Risks, and Complications
Sleep apnea is a potentially serious sleep disorder characterized by repeated pauses in breathing during sleep. If you snore loudly and feel tired even after a full night’s sleep, you may have sleep apnea.
Types of Obstructive Sleep Apnea (OSA)
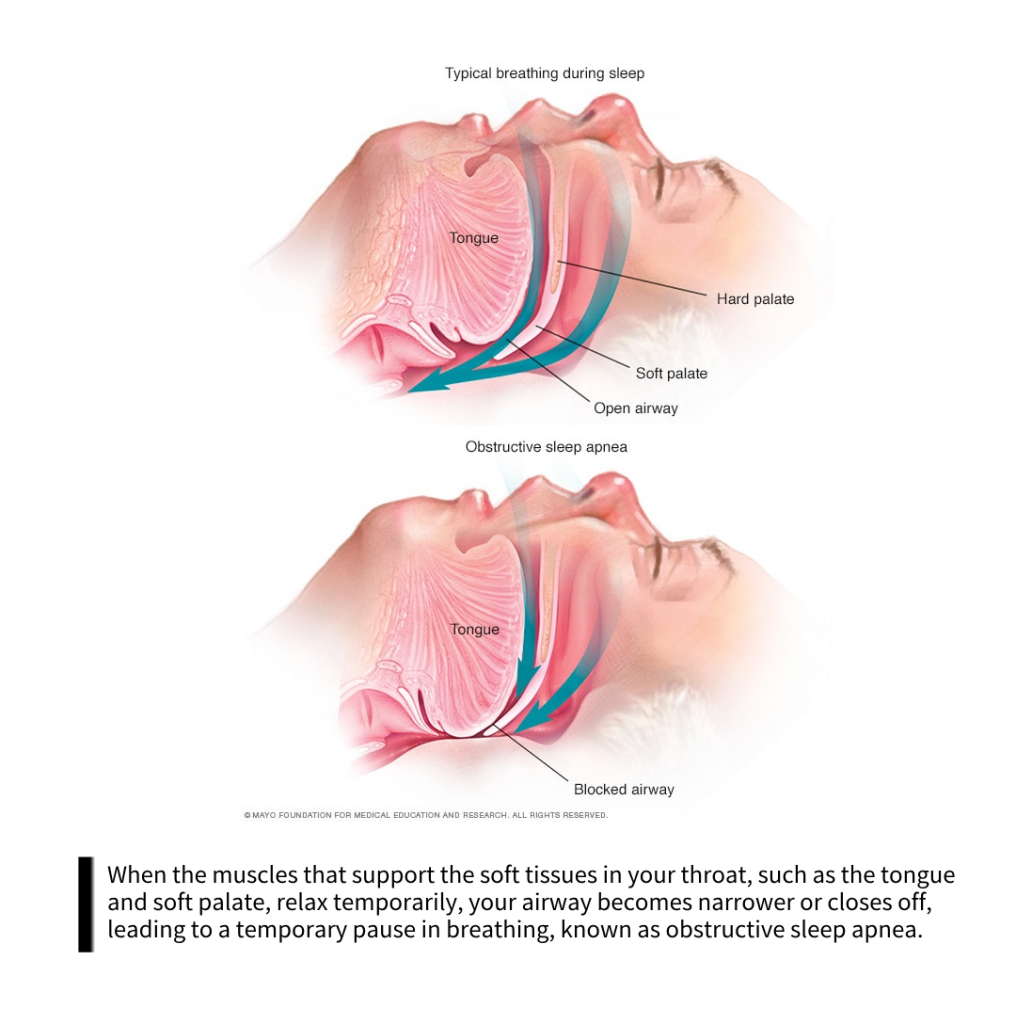
Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA) are the two main types of sleep apnea, with OSA being the more common form. It occurs when the muscles in the throat relax and block the airway, preventing air from flowing into the lungs. These muscles support the soft palate, the triangular tissue hanging from the soft palate (uvula), the tonsils, the side walls of the throat, and the tongue. If these muscles relax, the airway narrows or closes during inhalation. This results in inadequate air intake, leading to a decrease in oxygen levels in the blood. When your brain detects the inability to breathe, it temporarily arouses you to reopen the airway. You may snore, choke, or gasp during this process. These arousals are often brief, and you may not even remember them. If this pattern repeats 5-30 times or more per hour and continues throughout the night, it can make it difficult for you to enter into restful deep sleep stages.
Symptoms of Obstructive Sleep Apnea (OSA)
The symptoms of obstructive sleep apnea (OSA) and central sleep apnea often overlap, making it difficult to determine which type you may have. Common symptoms of both obstructive and central sleep apnea include:
- Loud snoring.
- Pauses in breathing during sleep (noticed by others).
- Gasping for air during sleep.
- Waking up with a dry mouth.
- Morning headaches.
- Difficulty maintaining continuous sleep (insomnia).
- Excessive daytime sleepiness (hypersomnia).
- Difficulty concentrating while awake.
- Irritability.
Risk Factors for Obstructive Sleep Apnea (OSA)
- Overweight or Obesity: Obesity significantly increases the risk of OSA. Fat deposits around the upper airway can obstruct breathing.
- Neck Circumference: People with thicker necks may have narrower airways.
- Narrowed Airway: You may inherit a narrow throat or have enlarged tonsils or adenoids, which can block the airway, especially in children.
- Gender: Men are two to three times more likely to have sleep apnea than women. However, the risk for women increases if they are overweight or postmenopausal.
- Advanced Age: Sleep apnea is more common in older adults.
- Family History: Having family members with sleep apnea may increase your risk.
- Alcohol, Sedatives, or Tranquilizers: These substances relax throat muscles, worsening obstructive sleep apnea.
- Smoking: Smokers are three times more likely to have obstructive sleep apnea than nonsmokers. Smoking exacerbates upper airway inflammation and fluid retention.
- Nasal Congestion: If you have difficulty breathing through your nose due to structural issues or allergies, you are more likely to have obstructive sleep apnea.
- Medical Conditions: Congestive heart failure, hypertension, and type 2 diabetes are some medical conditions that may increase the risk of developing obstructive sleep apnea. Conditions such as polycystic ovary syndrome, hormonal disorders, previous stroke, and chronic lung diseases like asthma can also increase the risk of developing sleep apnea.
Potential Complications of Obstructive Sleep Apnea (OSA)
- Daytime Fatigue: Frequent arousals associated with sleep apnea prevent restorative sleep, leading to excessive daytime sleepiness, fatigue, and irritability. Patients may struggle to concentrate and may even fall asleep during activities like working, watching TV, or driving. This increases the risk of accidents and work-related injuries. Additionally, mood swings, irritability, or depression may occur. Children and adolescents with sleep apnea may exhibit poor performance or behavioral issues at school.
- Hypertension or Heart Disease: Drops in blood oxygen levels during OSA episodes can elevate blood pressure and strain the cardiovascular system. OSA increases the risk of developing hypertension. It may also increase the risk of recurrent heart attacks, stroke, and cardiac arrhythmias such as atrial fibrillation. For individuals with existing heart disease, recurrent episodes of low oxygen (hypoxia or hypoxemia) may trigger sudden death due to arrhythmias.
- Type 2 Diabetes: Sleep apnea increases the risk of insulin resistance and type 2 diabetes.
- Metabolic Syndrome: This condition (including high blood pressure, abnormal cholesterol levels, elevated blood sugar, and increased waist circumference) increases the risk of heart disease.
- Medication and Surgical Complications: Certain medications and general anesthesia can exacerbate obstructive sleep apnea. Sleep apnea patients are more likely to experience complications after major surgeries due to increased risk of respiratory problems, especially when sedated and lying flat.
- Liver Problems: Sleep apnea patients are more likely to have abnormal liver function tests, and their livers are more prone to signs of scarring (nonalcoholic fatty liver disease).
- Partner Sleep Disturbance: Loud snoring can disrupt the sleep of those around you. It’s not uncommon for partners to have to sleep in separate rooms or on different floors to get a good night’s rest.
OSA Diagnosis and Treating
Diagnosis of OSA
You may be referred to a sleep disorders center where medical professionals will assess your symptoms and sleep history (which you may provide with the assistance of a bed partner or family member, if possible). Further evaluation may involve monitoring your breathing and other physiological functions during sleep, such as heart rate, blood oxygen levels, cardiac, pulmonary, and brain activity, breathing patterns, as well as movements of your arms and legs, with equipment.

Solutions for OSA: Effective Devices and Surgical Options
For mild cases of sleep apnea, medical professionals may only recommend lifestyle changes such as weight loss or smoking cessation. Adjustments to your sleeping position may be necessary. If you have allergic rhinitis, treatment may be recommended.
If these measures fail to improve your symptoms or if your sleep apnea is moderate to severe, various other treatment methods may be considered.Some devices can help open the blocked airway. In other cases, surgery may be necessary.
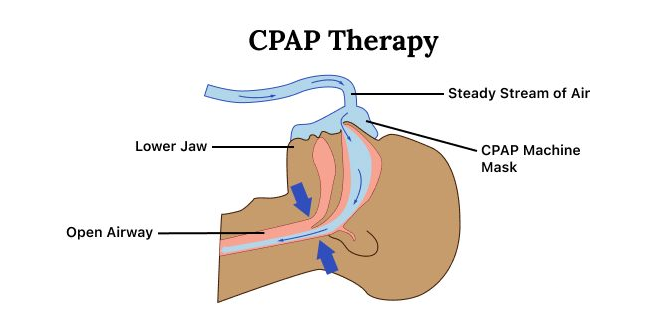
Continuous Positive Airway Pressure (CPAP): If you have moderate to severe obstructive sleep apnea, using a machine that delivers air pressure through a mask during sleep may be beneficial. With CPAP, the pressure is slightly higher than the surrounding air pressure, enough to keep your upper airway open and prevent apneas and snoring. While CPAP is the most common and reliable treatment for sleep apnea, some find it cumbersome or uncomfortable, and it can be costly, leading them to forgo its use. However, in practice, most people learn to adjust the tension of the straps on the mask for a comfortable and secure fit.
Other Airway Pressure Devices: If using a CPAP machine consistently poses a challenge, another type of airway pressure device that automatically adjusts pressure during sleep (auto CPAP) may be used. Devices that provide bilevel positive airway pressure (BPAP) are also available. These devices deliver higher pressure during inhalation and lower pressure during exhalation.
Oral Appliances: Another option is wearing an oral appliance to keep the throat open. While CPAP is more reliable and effective than oral appliances, they may be easier to use. Some products advance the lower jaw to open the throat, which can sometimes alleviate snoring and mild obstructive sleep apnea.

Dentists can utilize various devices. You may need to try different devices to find the right one. Once you find the suitable type, you will need to follow up with your dentist repeatedly during the first year, and then schedule regular follow-up appointments to ensure that the device still fits you well and to reassess your symptoms.
Surgery for Obstructive Sleep Apnea (OSA)
Patients with OSA may opt for surgery, but it is usually considered only after other treatments have failed. Before considering surgery, it is typically advised to try other treatment options for at least three months. However, surgery may be a good first-choice option for a minority of patients with certain jaw structure issues.
Surgical options may include:
- Tissue Removal: Surgeons remove tissue from the back of the mouth and the top of the throat during surgery (uvulopalatopharyngoplasty). Tonsils and adenoids may also be removed. This type of surgery may help prevent vibration of throat structures and treat snoring. Its effectiveness is not as reliable as CPAP and is not considered a definitive treatment for obstructive sleep apnea.
- Radiofrequency Energy: If patients cannot tolerate CPAP or oral appliances, using radiofrequency energy (radiofrequency ablation) to remove tissue deep in the throat is an alternative option.
- Tissue Shrinking: Shrinking tissue in the back of the mouth and deep in the throat with radiofrequency ablation is another option. This surgery may be suitable for mild to moderate sleep apnea. One study found that this method has similar outcomes to tissue removal but with lower surgical risks.
- Jaw Repositioning: In this medical procedure, the jawbone is moved forward relative to other facial bones. This can enlarge the space behind the tongue and soft palate, reducing the likelihood of blockage. Also known as maxillomandibular advancement surgery.
- Implants: Under local anesthesia, doctors surgically implant rods (typically made of polyester or plastic) into the soft palate. More research is needed to determine the efficacy of implants.
- Nerve Stimulation: This involves surgically inserting a stimulator into the nerve (hypoglossal nerve) that controls tongue movement. Increasing stimulation helps keep the tongue in a position that keeps the airway open. More research is needed.
- Creation of a New Breathing Passage (Tracheostomy): If other treatments have been unsuccessful and severe sleep apnea poses a life-threatening risk, this form of surgery may be necessary. During the surgery, surgeons make an incision in your neck and insert a metal or plastic tube for breathing.The stoma needs to be covered during the day and opened at night to allow air to bypass the blocked throat and enter the lungs.
There are also other surgeries that may help reduce snoring and assist in the treatment of sleep apnea by clearing or widening the airway:
- Tonsillectomy or Adenoidectomy: Removal of enlarged tonsils or adenoids.
- Weight Loss Surgery (Bariatric Surgery).
Lifestyle and Home Remedies
In some cases, obstructive sleep apnea and central sleep apnea can be managed through self-care. Here are some suggestions to try:
- Lose excess weight: Even a slight weight reduction may help alleviate throat constriction. In some cases, resolving to a healthy weight can alleviate sleep apnea, but weight regain may cause a recurrence.
- Exercise: Regular physical activity can help alleviate symptoms of obstructive sleep apnea, even without weight loss. Aim for 30 minutes of moderate exercise, such as brisk walking, most days of the week.
- Avoid alcohol and medications: Alcohol and certain medications like sedatives and sleeping pills can relax muscles at the back of the throat, disrupting breathing.
- Adjust sleep position: Sleep on your side or stomach rather than your back. Sleeping on your back can cause the tongue and soft palate to collapse against the back of the throat, blocking the airway. To prevent rolling onto your back during sleep, consider placing a tennis ball behind your pajamas or using commercial devices that emit vibrations when you shift positions during sleep.
- Quit smoking: If you smoke, seek resources to help you quit.
Go2sleep + M2 Enhancing Your Sleep Experience Now
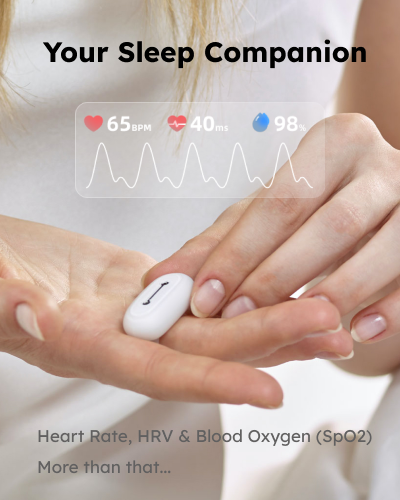
Go2sleep, an advanced sleep tracker with Heart Rate, HRV & Blood Oxygen (SpO2) Report / CSV Exportation .2024 Best Reports Sleep Tracker from Sleep Foundation is like a sleep lab in your hand, it helps you better understand your body and improve your sleep with daily feedback.
M2 is a quickly tailored oral appliance solution for those who are seeking to address snoring or mild OSA without medical assistance. FDA Cleared 4-Week Procedure,Refund Guarantee, Silent nights from Day One, adaptation in a Week, renew your life in a Month!or your money back!
Opt for the Go2sleep Tracker and M2 Anti-Snoring Device for Improved Sleep Management. Save More with our Bundle Offer. Only need $129, Save $69 , Buy Now !
ALL ARTICLES
Subscribe Us
Products
Company
Copyright © SLEEPON. All rights reserved.
SLEEPON keeps both Sleeponhealth and Sleepon.us due to the brand upgrading. We promise to provide the same products and service in both sites.







Leave a Reply